Dr. Clare Gerada, chair of the Royal College of GPs is in the news today. She warns that the Health and Social Care / Destroy the NHS Bill is damaging the relationship of trust between GPs and patients, warns of a two-tier health system run like a budget airline and suggests that GP practices should explore alternative models of organisation to GP partnerships.
NHS cuts
SMEs are concerned at the ConDem govenment’s destruction of the NHS and nasty changes to the welfare benefits system.
Private doctors treat healthier patients.
Medical students…
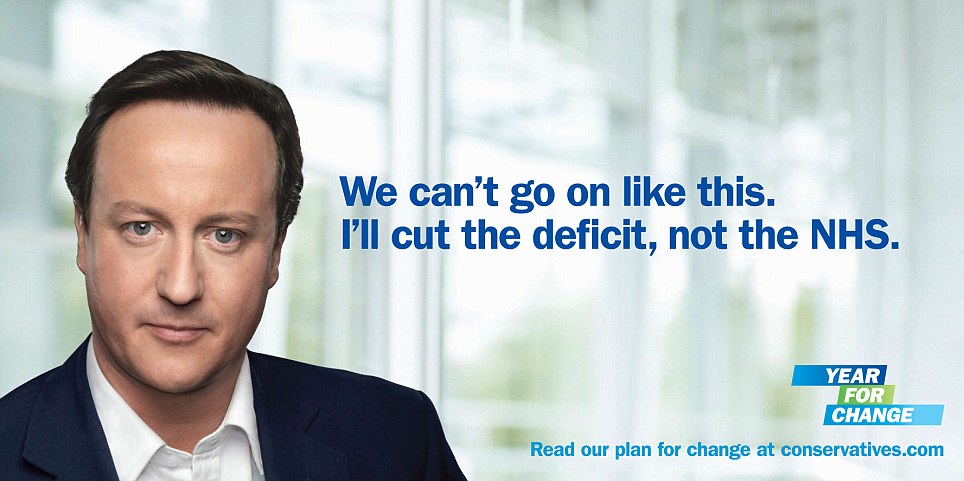
- Conservative election poster 2010
A few recent news articles about the UK’s Conservative and Liberal-Democrat (Conservative) coalition government – the ConDem’s – brutal attack on the National Health Service.
NHS bill threatens trust in GPs, says doctors’ leader | Society | The Guardian
NHS bill will lead to situation where healthcare is like budget airline with limited seats, says chair of Royal College of GPs
The NHS shake-up risks wrecking GPs’ relationship with their patients by turning them into rationers of care who deny the sick the treatment they need, warns the chair of the Royal College of GPs.
Family doctors could be “compromised” by having to decide between providing sick patients with the best possible treatment or meeting financial targets, according to Dr Clare Gerada.
Giving GPs control of health budgets, the cornerstone of health secretary Andrew Lansley’s restructuring of the NHS in England, could diminish the trust between patients and family doctors, she will tell the college’s annual conference.
“We must not risk long-term benefits being sacrificed in favour of short-term savings,” Gerada will tell the audience of 1,500 GPs in Liverpool. “How soon will it be, for example, before we stop referring for cochlear implant? An expensive intervention but one that in the long term saves enormous amounts of public money. But not a saving from our budget.
“How long will it be before we find ourselves injecting a patient’s knee joint – at Injections-R-us PLC – instead of referring to an orthopaedic surgeon for a knee replacement?”
In a detailed critique of Lansley’s health and social care bill, she will warn that: “As doctors we risk being compromised. We’ll have to choose between the best interests of our patients and those of the commissioning group’s purse. And, to make matters worse, we’ll also be rewarded for staying in budget – and not spending the money on restoring the child’s hearing. Now that’s what I call a perverse incentive.”
Her warning reflects widespread concern among doctors that exercising their financial responsibilities will lead some patients to believe they have been refused treatment on grounds of cost.
Lansley’s reforms also threaten to create a two-tier health service where the well-off can beat queues by paying for fast treatment as private patients in NHS hospitals, because of the proposed easing of the amount which foundation trust hospitals can earn from that source.
“I worry we’re heading towards a situation where healthcare will be like a budget airline. There will be two queues: one queue for those who can afford to pay, and another for those who can’t. Seats will be limited to those who muscle in first, and the rest will be left stranded on the tarmac.”
The British Medical Association, which represents hospital doctors as well as GPs, said it shared Gerada’s concerns.
“In general, we would agree with Clare Gerada’s comments about the impact of the health and social care bill. The BMA has concerns about the conflicts of interest inherent in the bill as well as the effects of the market on healthcare, and her comments fit with the views of most doctors,” said a spokeswoman for the BMA, which wants the bill withdrawn or substantially amended.
A Department of Health spokesperson said: “The NHS is not for sale and this government is committed to a real terms increase in funding for it. We want to give GPs the power and control to make the right decisions on behalf of their patients.
“Talk of budget airlines is nonsense pure and simple. In the new NHS, everyone will fly first class. Quality will improve as both patients and frontline staff are able to make choices.
…
…
When I come home from work and my son asks me what sort of day I’ve had, on a good day I want to be able to say “I saved a life”, not “I met a budget”.
Of course, it’s important that GPs are mindful of resources. We have a responsibility to spend the public’s money carefully and wisely. That goes without saying.
But we must never lose sight of the patient as a person, at the heart of our practice. Patients are not “commodities” to be bought and sold in the health marketplace.
In this brave new cost-driven, competitive, managed-care world, I worry about the effect the language of marketing is having on our clinical relationships.
It’s changing the precious relationship between clinician and patient into a crudely costed financial procedure. Turning our patients into aliquots of costed tariffs and us into financial managers of care.
We are already embracing the language of the market when we talk about, for example, care pathways, case management, demand management, productivity, clinical and financial alignment, risk stratification.
We’re already accused of making “inappropriate referrals” whenever we put what’s best for our patients above what’s best for saving money.
We’re being forced to comply with referral protocols and so-called rules-based medicine, in an effort to control medical care before it’s delivered.
Referral management systems – already widespread – place a hidden stranger in the consulting room. A hidden stranger who interferes with decisions that should be made by GPs in partnership with their patients.
Insulting terms, like “frequent flyers”, are being used to describe people who are sick and need our care and attention.
The archbishop of Canterbury attacked what he described as “the quiet resurgence of the seductive language of the deserving and undeserving poor”. If we don’t watch out, the deserving and undeserving poor could soon be joined by the deserving and undeserving sick.
I worry we’re heading towards a situation where healthcare will be like a budget airline. There’ll be two queues: one queue for those who can afford to pay, and another for those who can’t. Seats will be limited to those who muscle in first. And the rest will be left stranded on the tarmac.
This can’t be right. After all, no one chooses to be sick. We must hold fast to the principle that good healthcare should be available to all, regardless of wealth.
…
Gerada: We need to move on from GP partnerships – Pulse
GPs need to forget about the partnership model and look at new models of organising their practices, such as federations, says RCGP chair Dr Clare Gerada.
In a sometimes heated discussion over the lack of partnership opportunities for salaried GPs, Dr Gerada urged GPs to stop talking about the partner/salaried divide, saying that model belonged to the last century.
Delegates attending a ‘Partnership Debate’ at the RCGP annual conference backed a motion that the profession was doing new GPs ‘a disservice with a lack of partnership opportunities’, but RCGP leaders urged the profession to think more laterally about how the profession is organised.
Dr Gerada, a GP in Kennington whose practice employs around 100 salaried GPs, admitted the partnership debate was ‘complex’ but argued that a ‘new model’ of general practice was needed in the 21st Century.
She said: ‘I think we should stop talking about the salaried/partnership divide. I think we should start talking about federating – joining and collaborating across practices, sharing expertise and resources.’
‘While the partnership model may be the model for the 20th Century I think we need to move on and find a new model.’
…
Pontefract Hospital A&E will close overnight – Lifestyle – Pontefract Express
NIGHT time closure of Pontefract Hospital’s A&E department will start next month, it has been decided today (Thursday October 20).
At a public meeting of the Mid Yorkshire Hospitals NHS Trust all but one member of the board voted in favour of proposals which will see the unit shut from 10pm to 8am from November 1.
At the meeting at Pinderfields Hospital, Wakefield, the trust said the closure was due to staffing levels, adding if enough doctors at the right level could be recruited the opening hours would be reassessed.
…
SMEs fear cost of NHS and welfare reforms – IFAonline
More than half of SME employers fear the cost impact of the government’s health and welfare reforms, according to Jelf Group.
As a result it called for the House of Lords to help prevent potentially severe consequences and examine the effects on business of the new regimes.
The employee benefits intermediary conducted a poll of 169 SME businesses at a recent seminar and found 55% worried about the reform’s implications.
It suggested the main reasons that employers were fearful of increased financial pressures came from government overhauls of the NHS and welfare systems.
“Anecdotal evidence of increased waiting lists on the NHS may mean key employees take longer to return to the workplace,” it said.
“In the current economic climate this could be catastrophic for marginally profitable employers and even worse for fledgling business yet to make a return.
…
Management in Practice – Private sector ‘treats healthier patients’
Patients seen in independent sector treatment centres (ISTCs) tend to be younger, in better health and from “far more affluent areas” than those seen by NHS hospitals, research suggests.
The research, published in the British Medical Journal, also shows patients undergoing surgery in ISTCs had “slightly better outcomes” than patients treated in NHS centres.
However, the researchers claim such differences are “minor” and “unlikely to be clinically significant”.
The researchers, led by Professor Jan van der Meulen at the London School of Hygiene and Tropical Medicine, claims the study proves ISTCs treat patients with a more “favourable mix case profile”.
Yet, they also claim the results of their research “lessons concerns that ISTCs are ‘cherry picking’ the healthiest patients.”
“Our findings support the idea that separating elective surgical care from emergency services could improve the quality of care,” said the researchers.
…